A prior authorization delay occurs when payer approval for a test, procedure, or medication stalls due to missing documentation, payer requirements, or unanswered requests.
For large healthcare organizations, these delays are more than an inconvenience. A single oversight in one clinic can ripple across multiple sites, slowing care delivery, straining staff capacity, and disrupting financial performance.
In 2022, 7.4% of prior authorizations were denied—often for avoidable reasons such as incomplete or inconsistent submissions (KFF, 2024). At scale, these inefficiencies reduce patient throughput, increase burnout, and threaten revenue stability.
Why Prior Authorization Delays Happen
Authorization slowdowns often trace back to small but critical workflow gaps:
- Incomplete documentation – Missing chart notes, test results, or coding details.
- Missed payer requirements — Overlooking prior labs, referrals, or consult notes.
- Communication gaps – Insurer requests left unanswered, causing stalls.
Individually, these gaps are manageable. Across high patient volumes and multiple sites, they create bottlenecks that slow entire health systems.
Strategies to Reduce Prior Authorization Delays
Enterprise organizations are turning to Virtual Medical Assistants (VMAs) to build operational discipline at scale. By embedding repeatable workflows, VMAs create consistency and accountability across locations:
- Verify coverage early — Confirm insurance before appointments.
- Collect payer-specific documentation — Gather requirements up front, reducing back-and-forth.
- Apply standardized checklists — Reduce oversights across payers.
- Maintain audit trails — Timestamp every request and follow-up.
- Schedule proactive follow-ups — Keep requests from stalling.
- Prepare appeals in advance — Resolve denials quickly with complete documentation.
This structured approach transforms prior authorization from a reactive burden into a controlled, trackable, and scalable process.
What Are the Results at Scale?
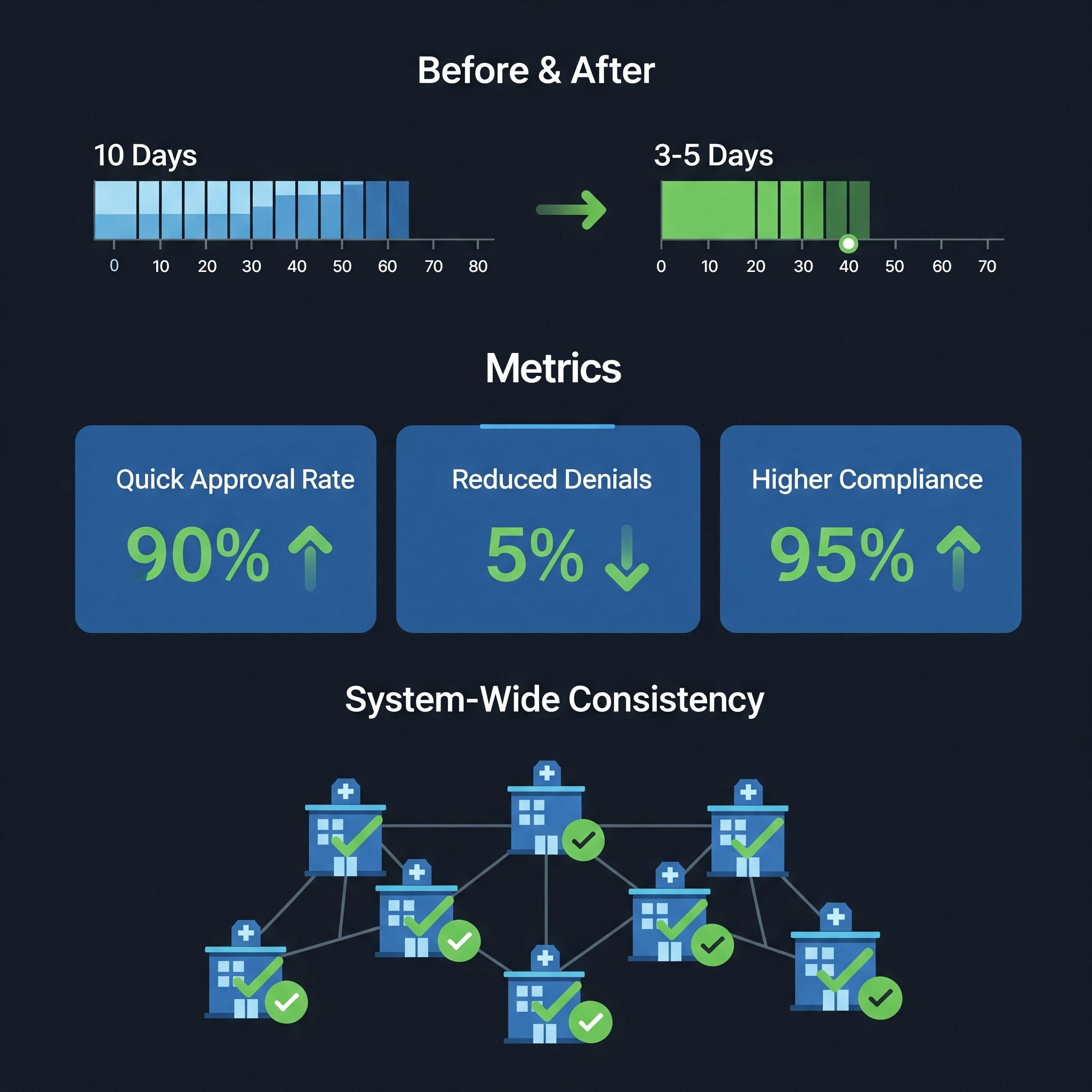
Health systems applying structured workflows have reduced turnaround times from 10 days to 3–5 days. At scale, this delivers measurable benefits:
- Faster patient access — Approvals keep care schedules on track.
- Operational consistency — Standardized processes deliver reliable outcomes across all sites and specialties.
- Compliance strength — Clear audit trails reduce payer disputes and strengthen compliance posture.
- Staff optimization — Clinicians spend more time on patient care, less on admin backlogs.
- Financial resilience — Reduced denials and faster approvals protect revenue.
Moving Forward
Prior authorization doesn’t have to remain a choke point in healthcare operations. With structured, repeatable workflows, health systems can accelerate approvals, reduce denials, and strengthen compliance, building both operational resilience and patient access.
A recent case study illustrates this impact: one provider network cut approval times in half by embedding standardized authorization workflows managed by VMAs, ensuring both speed and payer trust at scale.
References:
https://www.medicarerights.org/medicare-watch/2024/09/26/medicare-advantage-denials-increased-before-the-implementation-of-new-prior-authorization-rules?
https://www.aafp.org/pubs/fpm/issues/2006/0600/p45.html?





